Mapping The Gaps: Understanding Medically Underserved Areas And Their Impact
Mapping the Gaps: Understanding Medically Underserved Areas and Their Impact
Related Articles: Mapping the Gaps: Understanding Medically Underserved Areas and Their Impact
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to Mapping the Gaps: Understanding Medically Underserved Areas and Their Impact. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Mapping the Gaps: Understanding Medically Underserved Areas and Their Impact

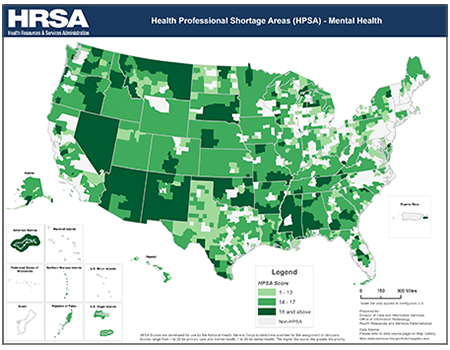
The concept of "medically underserved areas" (MUAs) encompasses regions facing significant challenges in accessing quality healthcare. These areas often exhibit a scarcity of healthcare providers, limited healthcare infrastructure, and socioeconomic factors that hinder individuals from receiving necessary medical care. Recognizing and addressing these disparities is crucial for ensuring equitable healthcare access and improving public health outcomes.
Defining Medically Underserved Areas:
The identification of MUAs is a complex process involving various factors, including:
- Provider-to-Population Ratio: A low ratio of healthcare professionals, such as physicians, nurses, and dentists, per capita indicates a shortage of medical personnel.
- Poverty Rate: High poverty rates often correlate with limited access to healthcare due to financial constraints and lack of health insurance.
- Infant Mortality Rate: Elevated infant mortality rates can signal inadequate prenatal care and overall healthcare access.
- Lack of Transportation: Limited access to reliable transportation systems can hinder individuals from reaching healthcare facilities, particularly in rural areas.
- Health Status Indicators: Poor health outcomes, such as high rates of chronic diseases and preventable conditions, can be indicative of inadequate healthcare access.
The Significance of Medically Underserved Area Maps:
Medically underserved area maps serve as vital tools for understanding the distribution of healthcare access across geographical regions. They provide a visual representation of areas facing disparities in healthcare provision, allowing policymakers, healthcare providers, and researchers to:
- Identify Areas of Need: Maps highlight regions experiencing a shortage of healthcare professionals, inadequate infrastructure, and limited access to essential services.
- Target Resources: By pinpointing areas with the greatest need, policymakers can allocate resources effectively to expand healthcare access and improve health outcomes.
- Develop Strategies for Improvement: Maps facilitate the development of targeted interventions, such as building new healthcare facilities, increasing the number of healthcare professionals, and enhancing transportation infrastructure.
- Monitor Progress: Tracking changes in the distribution of healthcare resources over time allows for the evaluation of the effectiveness of interventions and the identification of areas requiring further attention.
- Promote Collaboration: Maps foster collaboration among healthcare stakeholders, encouraging the sharing of resources and expertise to address healthcare disparities.
Types of Medically Underserved Area Maps:
Various types of maps are used to depict medically underserved areas, each focusing on specific aspects of healthcare access:
- Provider Density Maps: These maps illustrate the distribution of healthcare providers, such as physicians, nurses, and dentists, across a geographical region. Areas with low provider density are considered medically underserved.
- Population-to-Provider Ratio Maps: These maps display the ratio of population to healthcare providers, highlighting areas with a high population-to-provider ratio, indicating limited access to healthcare services.
- Health Status Maps: These maps depict the prevalence of specific health conditions, such as chronic diseases or preventable conditions, within a region. Areas with high rates of these conditions may indicate a lack of access to preventive care and healthcare services.
- Socioeconomic Maps: These maps illustrate socioeconomic factors, such as poverty rates, education levels, and unemployment rates, that can influence access to healthcare. Areas with high socioeconomic vulnerability are often associated with limited healthcare access.
Benefits of Using Medically Underserved Area Maps:
- Improved Healthcare Planning: Maps provide valuable data for healthcare planners, enabling them to identify areas requiring increased healthcare resources and develop strategies for improving access.
- Enhanced Resource Allocation: By highlighting regions with the greatest need, maps facilitate the efficient allocation of resources, ensuring that healthcare services reach those who require them most.
- Targeted Interventions: Maps enable the development of targeted interventions, such as mobile clinics, telemedicine services, and community health programs, to address specific healthcare needs in underserved areas.
- Public Health Surveillance: Maps provide a valuable tool for public health surveillance, allowing for the monitoring of healthcare access and health outcomes over time.
- Community Empowerment: Maps can empower communities to advocate for improved healthcare access and hold policymakers accountable for addressing healthcare disparities.
Challenges in Using Medically Underserved Area Maps:
Despite their numerous benefits, medically underserved area maps also face certain challenges:
- Data Availability and Accuracy: The accuracy of maps depends on the availability of reliable data on healthcare providers, population demographics, and health status indicators. Data gaps and inconsistencies can limit the effectiveness of maps.
- Definition of Underserved: The definition of "medically underserved" can vary depending on the criteria used. Different organizations may have different thresholds for defining underserved areas, leading to discrepancies in map results.
- Complexity of Factors: Healthcare access is influenced by a complex interplay of factors, including socioeconomic conditions, cultural beliefs, and transportation infrastructure. Maps may not fully capture the nuances of these factors.
- Data Collection and Maintenance: Maintaining accurate and up-to-date data for maps requires ongoing efforts to collect and update information. This can be a resource-intensive process.
- Public Perception: Maps may be perceived as stigmatizing or blaming communities for their healthcare challenges. It is important to ensure that maps are used in a way that promotes understanding and collaboration rather than blame.
FAQs on Medically Underserved Area Maps:
Q: How are medically underserved areas identified?
A: Medically underserved areas are identified based on a combination of factors, including provider-to-population ratios, poverty rates, infant mortality rates, lack of transportation, and health status indicators.
Q: What are the limitations of medically underserved area maps?
A: Maps may not fully capture the complexity of factors influencing healthcare access, and data availability and accuracy can be challenging.
Q: How can medically underserved area maps be used to improve healthcare access?
A: Maps can help identify areas of need, target resources, develop strategies for improvement, and promote collaboration among healthcare stakeholders.
Q: What are some examples of interventions that can be implemented in medically underserved areas?
A: Interventions include building new healthcare facilities, increasing the number of healthcare professionals, enhancing transportation infrastructure, providing mobile clinics, and implementing telemedicine services.
Q: How can communities be empowered to advocate for improved healthcare access?
A: Maps can provide communities with data to support their advocacy efforts and hold policymakers accountable for addressing healthcare disparities.
Tips for Using Medically Underserved Area Maps:
- Use multiple data sources: Combine data from various sources to create a comprehensive picture of healthcare access.
- Consider context: Understand the specific factors influencing healthcare access in each area.
- Engage with communities: Collaborate with communities to ensure that maps are used in a way that is sensitive and beneficial.
- Monitor progress: Track changes in healthcare access over time to evaluate the effectiveness of interventions.
- Promote collaboration: Encourage collaboration among healthcare stakeholders to address healthcare disparities.
Conclusion:
Medically underserved area maps are invaluable tools for understanding and addressing healthcare disparities. By providing a visual representation of areas facing challenges in accessing quality healthcare, these maps enable policymakers, healthcare providers, and researchers to identify areas of need, target resources, develop strategies for improvement, and monitor progress. However, it is important to acknowledge the limitations of maps and use them in conjunction with other data sources and community engagement to ensure that they are used effectively to promote equitable healthcare access for all.







Closure
Thus, we hope this article has provided valuable insights into Mapping the Gaps: Understanding Medically Underserved Areas and Their Impact. We hope you find this article informative and beneficial. See you in our next article!